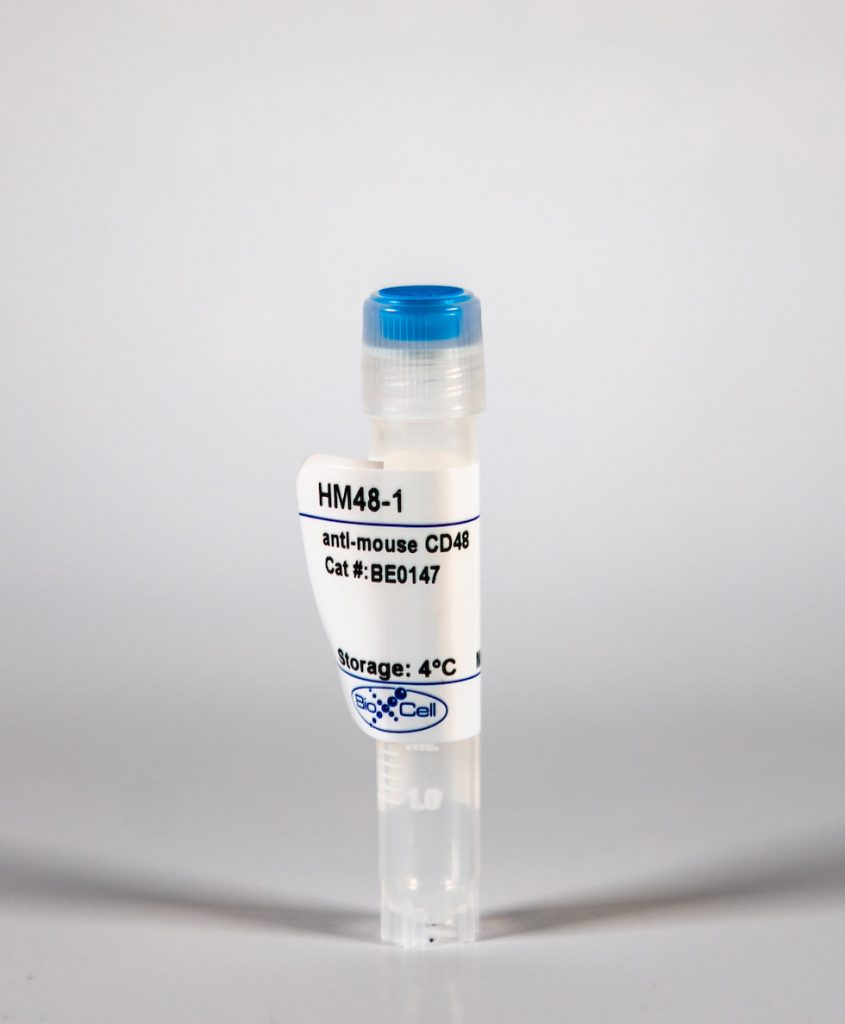
InVivoMab anti-mouse CD48
| Clone | HM48-1 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0147 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The HM48-1 monoclonal antibody reacts with mouse CD48 also known as BCM1, Blast-1 (human), and OX-45 (rat). CD48 is a 45 kDa GPI-anchored glycoprotein and a member of the SLAM family and Ig superfamily. CD48 is expressed on T and B lymphocytes as well as monocytes and macrophages. CD48 plays a critical role in adhesion and T cell activation. The primary ligands for CD48 are CD2 and CD244. The HM48-1 antibody is reported to block the CD48/CD2 and CD48/CD244 interactions in vivo as well as inhibit the proliferative response of mitogen-activated spleen cells, provide a co-stimulatory signal for activated T cells in vitro, and prolong cardiac allograft survival in vivo.
| Isotype | Armenian Hamster IgG |
| Recommended Isotype Control(s) | InVivoMAb polyclonal Armenian hamster IgG |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | MBL2 mouse T lymphoma cells |
| Reported Applications |
|
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_10949470 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
InVivoMAb anti-mouse CD48 (Clone: HM48-1)
Jing, W., et al. (2015). "Combined immune checkpoint protein blockade and low dose whole body irradiation as immunotherapy for myeloma." J Immunother Cancer 3(1): 2. PubMed
BACKGROUND: Multiple myeloma is characterized by the presence of transformed neoplastic plasma cells in the bone marrow and is generally considered to be an incurable disease. Successful treatments will likely require multi-faceted approaches incorporating conventional drug therapies, immunotherapy and other novel treatments. Our lab previously showed that a combination of transient lymphodepletion (sublethal whole body irradiation) and PD-1/PD-L1 blockade generated anti-myeloma T cell reactivity capable of eliminating established disease. We hypothesized that blocking a combination of checkpoint receptors in the context of low-dose, lymphodepleting whole body radiation would boost anti-tumor immunity. METHODS: To test our central hypothesis, we utilized a 5T33 murine multiple myeloma model. Myeloma-bearing mice were treated with a low dose of whole body irradiation and combinations of blocking antibodies to PD-L1, LAG-3, TIM-3, CD48 (the ligand for 2B4) and CTLA4. RESULTS: Temporal phenotypic analysis of bone marrow from myeloma-bearing mice demonstrated that elevated percentages of PD-1, 2B4, LAG-3 and TIM-3 proteins were expressed on T cells. When PD-L1 blockade was combined with blocking antibodies to LAG-3, TIM-3 or CTLA4, synergistic or additive increases in survival were observed (survival rates improved from ~30% to >80%). The increased survival rates correlated with increased frequencies of tumor-reactive CD8 and CD4 T cells. When stimulated in vitro with myeloma cells, CD8 T cells from treated mice produced elevated levels proinflammatory cytokines. Cytokines were spontaneously released from CD4 T cells isolated from mice treated with PD-L1 plus CTLA4 blocking antibodies. CONCLUSIONS: These data indicate that blocking PD-1/PD-L1 interactions in conjunction with other immune checkpoint proteins provides synergistic anti-tumor efficacy following lymphodepletive doses of whole body irradiation. This strategy is a promising combination strategy for myeloma and other hematologic malignancies.
Erickson, J. J., et al. (2014). "Programmed death-1 impairs secondary effector lung CD8(+) T cells during respiratory virus reinfection." J Immunol 193(10): 5108-5117. PubMed
Reinfections with respiratory viruses are common and cause significant clinical illness, yet precise mechanisms governing this susceptibility are ill defined. Lung Ag-specific CD8(+) T cells (T(CD8)) are impaired during acute viral lower respiratory infection by the inhibitory receptor programmed death-1 (PD-1). To determine whether PD-1 contributes to recurrent infection, we first established a model of reinfection by challenging B cell-deficient mice with human metapneumovirus (HMPV) several weeks after primary infection, and found that HMPV replicated to high titers in the lungs. A robust secondary effector lung TCD8 response was generated during reinfection, but these cells were more impaired and more highly expressed the inhibitory receptors PD-1, LAG-3, and 2B4 than primary T(CD8). In vitro blockade demonstrated that PD-1 was the dominant inhibitory receptor early after reinfection. In vivo therapeutic PD-1 blockade during HMPV reinfection restored lung T(CD8) effector functions (i.e., degranulation and cytokine production) and enhanced viral clearance. PD-1 also limited the protective efficacy of HMPV epitope-specific peptide vaccination and impaired lung T(CD8) during heterotypic influenza virus challenge infection. Our results indicate that PD-1 signaling may contribute to respiratory virus reinfection and evasion of vaccine-elicited immune responses. These results have important implications for the design of effective vaccines against respiratory viruses.