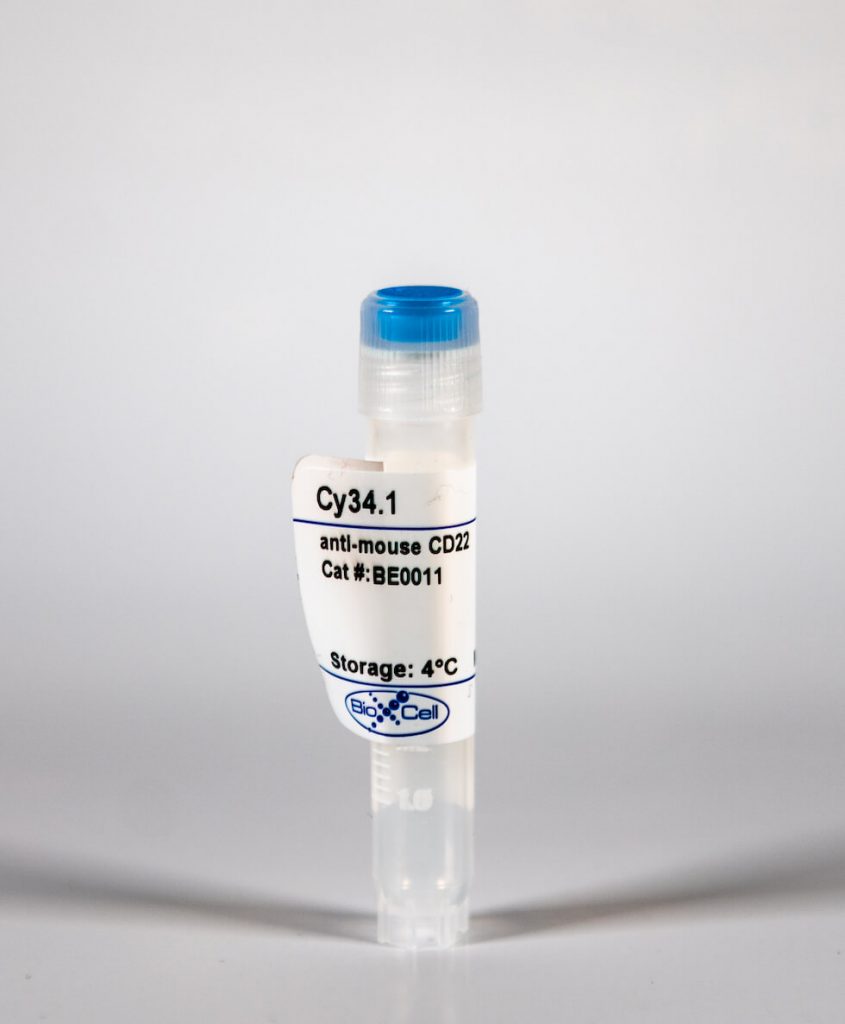
InVivoMAb anti-mouse CD22
| Clone | Cy34.1 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0011 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The Cy34.1 monoclonal antibody reacts with mouse CD22, a member of the SIGLEC family of lectins. CD22 is expressed at high levels on the surface of mature follicular and marginal zone B lymphocytes, B-1 cells, and plasma cells and associates with the B-cell antigen receptor. CD22 mediates B cell adhesion to ligands on endothelial cells in the bone marrow. Additionally, CD22 to negatively regulates B cell activation and prevents the development of autoimmune diseases. The Cy34.1 antibody has been shown to augment B cell proliferation in response to LPS or anti-mouse Ig µ chain.
| Isotype | Mouse IgG1, κ |
| Recommended Isotype Control(s) | InVivoMAb mouse IgG1 isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | B10.D2 mouse splenocytes |
| Reported Applications |
|
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_1107613 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
INVIVOMAB ANTI-MOUSE CD22 (CLONE: CY34.1)
Sawen, P., et al. (2016). “Mitotic History Reveals Distinct Stem Cell Populations and Their Contributions to Hematopoiesis.” Cell Rep 14(12): 2809-2818. PubMed
Homeostasis of short-lived blood cells is dependent on rapid proliferation of immature precursors. Using a conditional histone 2B-mCherry-labeling mouse model, we characterize hematopoietic stem cell (HSC) and progenitor proliferation dynamics in steady state and following several types of induced stress. HSC proliferation following HSC transplantation into lethally irradiated mice is fundamentally different not only from native hematopoiesis but also from other stress contexts. Whereas transplantation promoted sustained, long-term proliferation of HSCs, both cytokine-induced mobilization and acute depletion of selected blood cell lineages elicited very limited recruitment of HSCs to the proliferative pool. By coupling mCherry-based analysis of proliferation history with multiplex gene expression analyses on single cells, we have found that HSCs can be stratified into four distinct subtypes. These subtypes have distinct molecular signatures and differ significantly in their reconstitution potentials, showcasing the power of tracking proliferation history when resolving functional heterogeneity of HSCs.
Muller, J., et al. (2013). “CD22 ligand-binding and signaling domains reciprocally regulate B-cell Ca2+ signaling.” Proc Natl Acad Sci U S A 110(30): 12402-12407. PubMed
A high proportion of human B cells carry B-cell receptors (BCRs) that are autoreactive. Inhibitory receptors such as CD22 can downmodulate autoreactive BCR responses. With its extracellular domain, CD22 binds to sialic acids in alpha2,6 linkages in cis, on the surface of the same B cell or in trans, on other cells. Sialic acids are self ligands, as they are abundant in vertebrates, but are usually not expressed by pathogens. We show that cis-ligand binding of CD22 is crucial for the regulation of B-cell Ca(2+) signaling by controlling the CD22 association to the BCR. Mice with a mutated CD22 ligand-binding domain of CD22 showed strongly reduced Ca(2+) signaling. In contrast, mice with mutated CD22 immunoreceptor tyrosine-based inhibition motifs have increased B-cell Ca(2+) responses, increased B-cell turnover, and impaired survival of the B cells. Thus, the CD22 ligand-binding domain has a crucial function in regulating BCR signaling, which is relevant for controlling autoimmunity.
Wohner, M., et al. (2012). “Human CD22 cannot fully substitute murine CD22 functions in vivo, as shown in a new knockin mouse model.” Eur J Immunol 42(11): 3009-3018. PubMed
CD22, an inhibitory co-receptor of the B-cell receptor, shows a B-cell-specific expression pattern and is expressed on most B-cell lymphomas. The anti-CD22 antibody Epratuzumab is in clinical trials for B-cell non-Hodgkin lymphoma and systemic lupus erythematosus, but shows a mostly unknown mode of action. We generated a new mouse model that expresses human CD22 instead of murine CD22 (Huki CD22 mice), in which human CD22 can be targeted. Expression of human CD22 on the B cells of Huki CD22 mice does not generally interfere with B-cell development. However, Huki CD22 mice show a reduction of the population of mature recirculating B cells in the bone marrow and reduced transitional and marginal zone B cells in the spleen, phenotypes resembling that of CD22-deficient mice. Similarly, enhanced BCR-induced Ca(2+) signalling is observed in Huki CD22 mice, which also mount normal immune responses toward different classes of antigens. Huki CD22 B cells show a normal anti-hCD22 antibody-mediated endocytosis. In conclusion, human CD22 cannot fully substitute for murine CD22 functions, possibly due to the changed intracellular tail of the protein or due to lower expression levels. Huki CD22 mice are a valuable new model for both antibody- and immunotoxin-mediated targeting of human CD22.
Duong, B. H., et al. (2010). “Decoration of T-independent antigen with ligands for CD22 and Siglec-G can suppress immunity and induce B cell tolerance in vivo.” J Exp Med 207(1): 173-187. PubMed
Autoreactive B lymphocytes first encountering self-antigens in peripheral tissues are normally regulated by induction of anergy or apoptosis. According to the “two-signal” model, antigen recognition alone should render B cells tolerant unless T cell help or inflammatory signals such as lipopolysaccharide are provided. However, no such signals seem necessary for responses to T-independent type 2 (TI-2) antigens, which are multimeric antigens lacking T cell epitopes and Toll-like receptor ligands. How then do mature B cells avoid making a TI-2-like response to multimeric self-antigens? We present evidence that TI-2 antigens decorated with ligands of inhibitory sialic acid-binding Ig-like lectins (siglecs) are poorly immunogenic and can induce tolerance to subsequent challenge with immunogenic antigen. Two siglecs, CD22 and Siglec-G, contributed to tolerance induction, preventing plasma cell differentiation or survival. Although mutations in CD22 and its signaling machinery have been associated with dysregulated B cell development and autoantibody production, previous analyses failed to identify a tolerance defect in antigen-specific mutant B cells. Our results support a role for siglecs in B cell self-/nonself-discrimination, namely suppressing responses to self-associated antigens while permitting rapid “missing self”-responses to unsialylated multimeric antigens. The results suggest use of siglec ligand antigen constructs as an approach for inducing tolerance.
Efanov, A., et al. (2010). “CD5+CD23+ leukemic cell populations in TCL1 transgenic mice show significantly increased proliferation and Akt phosphorylation.” Leukemia 24(5): 970-975. PubMed
B-cell chronic lymphocytic leukemia (B-CLL) is the most common adult leukemia. Deregulation of the T-cell leukemia/lymphoma 1 (TCL1) oncogene in mouse B cells causes a CD5-positive leukemia similar to aggressive human B-CLLs. We recently reported that levels of TCL1 expression in B-CLL are regulated by miR-29 and miR-181 that target 3′ UTR of TCL1. To determine whether treatment with microRNAs targeting TCL1 can inhibit B-CLL in mice, we generated TCL1 transgenic mice using a construct containing the 3′ and 5′ UTRs of TCL1 under B-cell-specific Emicro promoter (Emicro-TCL1FL). At the age of 16-20 months, these mice showed B-CLL-like disease. Immunophenotyping revealed accumulation of CD5+CD23+B220+ population in spleens and lymph nodes. Our results show that CD5+CD23+ B-cell populations from Emicro-TCL1FL mice actively proliferate and show significantly increased levels of phospho-Akt. Emicro-TCL1FL mice showed immunological abnormalities similar to human B-CLL, including hypoimmunoglobulinemia, abnormal levels of cytokines and impaired immune response. These findings revealed biochemical and immunological similarities between Tcl1-driven B-CLL in mice and human B-CLL.