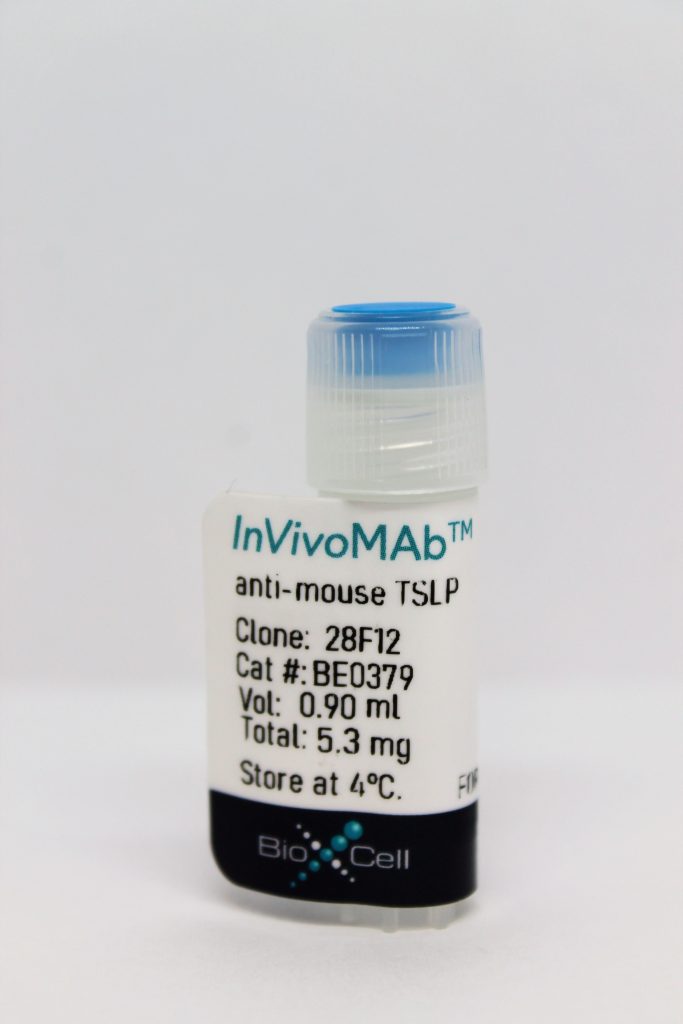
InVivoMAb anti-mouse TSLP
| Clone | 28F12 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0379 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The 28F12 monoclonal antibody reacts with mouse Thymic Stromal-Derived Lymphopoetin (TSLP). TSLP is a cytokine that is closely related to IL-7. TSLP is expressed predominantly by epithelial cells in the thymus, lung, skin, intestine, and tonsils, as well as stromal cells, mast cells, and dendritic cells. TSLP exerts its biological activities by binding to a heterodimeric receptor that consists of IL-7Rα and the TSLP receptor (TSLPR) chain. Expression of TSLP is regulated by NF-κB and can be induced by exposure to viral, bacterial, or parasitic products, inflammatory cytokines, and the Th2 cell–associated cytokines IL-4 and IL-13. TSLP has important roles in conditioning DCs to drive Th2 differentiation and its expression is increased in immunopathologies associated with dysregulated Th2 cell–type cytokine production, including atopic dermatitis and asthma. It has additionally been reported to promote antibody isotype class switching in B cells, to regulate the development of Foxp3+ Tregs in the human thymus, and to promote basophil hematopoiesis. The 28F12 antibody has been reported to inhibit the bioactivity of mouse TSLP in vivo and in vitro.
| Isotype | Rat IgG2a, κ |
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | Purified murine TSLP |
| Reported Applications |
|
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
INVIVOMAB ANTI-MOUSE TSLP
in vivo TSLP neutralization
Stier, M. T., et al. (2016). "Respiratory syncytial virus infection activates IL-13-producing group 2 innate lymphoid cells through thymic stromal lymphopoietin." J Allergy Clin Immunol 138(3): 814-824 e811. PubMed
BACKGROUND: Respiratory syncytial virus (RSV) is a major health care burden with a particularly high worldwide morbidity and mortality rate among infants. Data suggest that severe RSV-associated illness is in part caused by immunopathology associated with a robust type 2 response. OBJECTIVE: We sought to determine the capacity of RSV infection to stimulate group 2 innate lymphoid cells (ILC2s) and the associated mechanism in a murine model. METHODS: Wild-type (WT) BALB/c, thymic stromal lymphopoietin receptor (TSLPR) knockout (KO), or WT mice receiving an anti-TSLP neutralizing antibody were infected with the RSV strain 01/2-20. During the first 4 to 6 days of infection, lungs were collected for evaluation of viral load, protein concentration, airway mucus, airway reactivity, or ILC2 numbers. Results were confirmed with 2 additional RSV clinical isolates, 12/11-19 and 12/12-6, with known human pathogenic potential. RESULTS: RSV induced a 3-fold increase in the number of IL-13-producing ILC2s at day 4 after infection, with a concurrent increase in total lung IL-13 levels. Both thymic stromal lymphopoietin (TSLP) and IL-33 levels were increased 12 hours after infection. TSLPR KO mice did not mount an IL-13-producing ILC2 response to RSV infection. Additionally, neutralization of TSLP significantly attenuated the RSV-induced IL-13-producing ILC2 response. TSLPR KO mice displayed reduced lung IL-13 protein levels, decreased airway mucus and reactivity, attenuated weight loss, and similar viral loads as WT mice. Both 12/11-19 and 12/12-6 similarly induced IL-13-producing ILC2s through a TSLP-dependent mechanism. CONCLUSION: These data demonstrate that multiple pathogenic strains of RSV induce IL-13-producing ILC2 proliferation and activation through a TSLP-dependent mechanism in a murine model and suggest the potential therapeutic targeting of TSLP during severe RSV infection.
in vivo TSLP neutralization
Mosconi, I., et al. (2013). "Intestinal bacteria induce TSLP to promote mutualistic T-cell responses." Mucosal Immunol 6(6): 1157-1167. PubMed
Thymic stromal lymphopoietin (TSLP) is constitutively expressed in the intestine and is known to regulate inflammation in models of colitis. We show that steady-state TSLP expression requires intestinal bacteria and has an important role in limiting the expansion of colonic T helper type 17 (Th17) cells. Inappropriate expansion of the colonic Th17 cells occurred in response to an entirely benign intestinal microbiota, as determined following the colonization of germ-free C57BL/6 or TSLPR(-/-) mice with the altered Schaedler flora (ASF). TSLP-TSLPR (TSLP receptor) interactions also promoted the expansion of colonic Helios(-)Foxp3(+) regulatory T cells, necessary for the control of inappropriate Th17 responses following ASF bacterial colonization. In summary, these data reveal an important role for TSLP-TSLPR signaling in promoting steady-state mutualistic T-cell responses following intestinal bacterial colonization.
in vivo TSLP neutralization
in vitro TSLP neutralization
Sokol, C. L., et al. (2008). "A mechanism for the initiation of allergen-induced T helper type 2 responses." Nat Immunol 9(3): 310-318. PubMed
Both metazoan parasites and simple protein allergens induce T helper type 2 (TH2) immune responses, but the mechanisms by which the innate immune system senses these stimuli are unknown. In addition, the cellular source of cytokines that control TH2 differentiation in vivo has not been defined. Here we showed that basophils were activated and recruited to the draining lymph nodes specifically in response to TH2-inducing allergen challenge. Furthermore, we demonstrate that the basophil was the accessory cell type required for TH2 induction in response to protease allergens. Finally, we show that basophils were directly activated by protease allergens and produced TH2-inducing cytokines, including interleukin 4 and thymic stromal lymphopoietin, which are involved in TH2 differentiation in vivo.