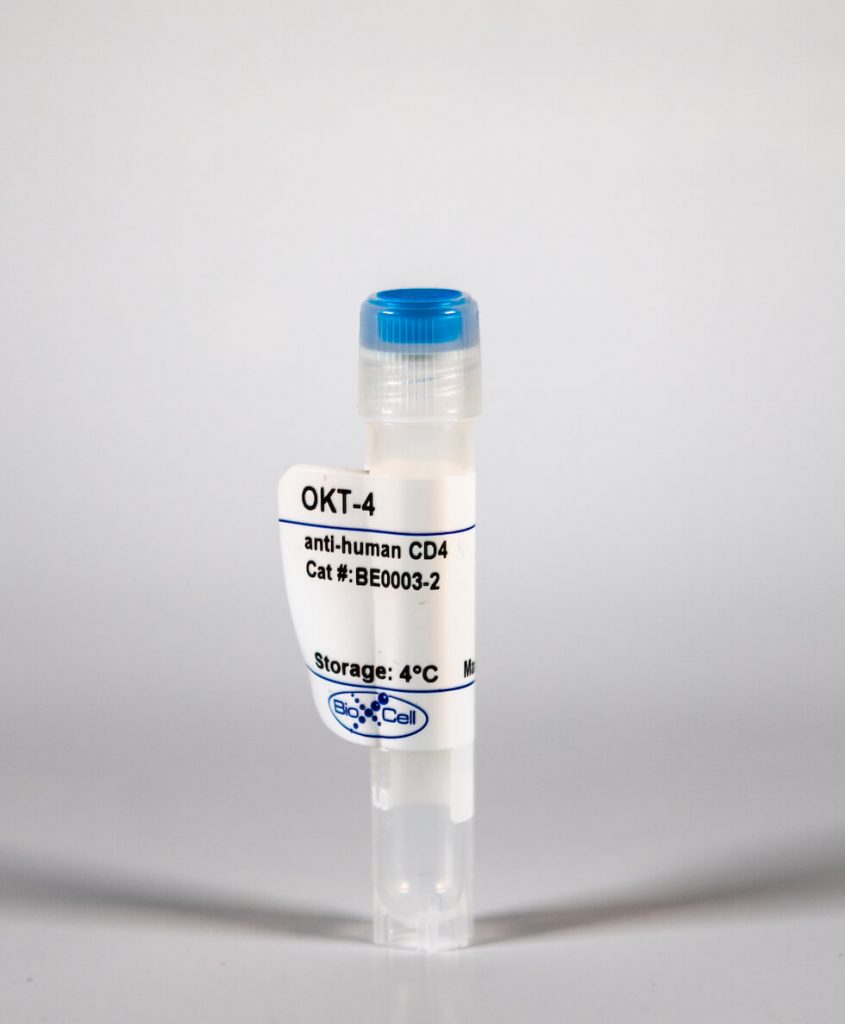
InVivoMAb anti-human CD4
| Clone | OKT-4 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0003-2 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The OKT-4 monoclonal antibody reacts with the human CD4. The CD4 antigen is a 55 kDa cell surface type I membrane glycoprotein belonging to the immunoglobulin superfamily. CD4 acts as a co-receptor which in cooperation with the T cell receptor (TCR) interacts with class II MHC molecules displayed by antigen presenting cells (APC). CD4 is expressed by the majority of thymocytes, most helper T cells, a subset of NK-T cells and weakly by dendritic cells and macrophages. CD4 plays an important role in the development of T cells and is required for mature T cells to function optimally.
| Isotype | Mouse IgG2b, κ |
| Recommended Isotype Control(s) | InVivoMAb mouse IgG2b isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | Human peripheral T cells |
| Reported Applications |
|
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_1107638 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
INVIVOMAB ANTI-HUMAN CD4 (CLONE: OKT-4)
Klammt, C., et al. (2015). “T cell receptor dwell times control the kinase activity of Zap70.” Nat Immunol 16(9): 961-969. PubMed
Kinase recruitment to membrane receptors is essential for signal transduction. However, the underlying regulatory mechanisms are poorly understood. We investigated how conformational changes control T cell receptor (TCR) association and activity of the kinase Zap70. Structural analysis showed that TCR binding or phosphorylation of Zap70 triggers a transition from a closed, autoinhibited conformation to an open conformation. Using Zap70 mutants with defined conformations, we found that TCR dwell times controlled Zap70 activity. The closed conformation minimized TCR dwell times and thereby prevented activation by membrane-associated kinases. Parallel recruitment of coreceptor-associated Lck kinase to the TCR ensured Zap70 phosphorylation and stabilized Zap70 TCR binding. Our study suggests that the dynamics of cytosolic enzyme recruitment to the plasma membrane regulate the activity and function of receptors lacking intrinsic catalytic activity.
Billerbeck, E., et al. (2013). “Characterization of human antiviral adaptive immune responses during hepatotropic virus infection in HLA-transgenic human immune system mice.” J Immunol 191(4): 1753-1764. PubMed
Humanized mice have emerged as a promising model to study human immunity in vivo. Although they are susceptible to many pathogens exhibiting an almost exclusive human tropism, human immune responses to infection remain functionally impaired. It has recently been demonstrated that the expression of HLA molecules improves human immunity to lymphotropic virus infections in humanized mice. However, little is known about the extent of functional human immune responses in nonlymphoid tissues, such as in the liver, and the role of HLA expression in this context. Therefore, we analyzed human antiviral immunity in humanized mice during a hepatotropic adenovirus infection. We compared immune responses of conventional humanized NOD SCID IL-2Rgamma-deficient (NSG) mice to those of a novel NOD SCID IL-2Rgamma-deficient strain transgenic for both HLA-A*0201 and a chimeric HLA-DR*0101 molecule. Using a firefly luciferase-expressing adenovirus and in vivo bioluminescence imaging, we demonstrate a human T cell-dependent partial clearance of adenovirus-infected cells from the liver of HLA-transgenic humanized mice. This correlated with liver infiltration and activation of T cells, as well as the detection of Ag-specific humoral and cellular immune responses. When infected with a hepatitis C virus NS3-expressing adenovirus, HLA-transgenic humanized mice mounted an HLA-A*0201-restricted hepatitis C virus NS3-specific CD8(+) T cell response. In conclusion, our study provides evidence for the generation of partial functional antiviral immune responses against a hepatotropic pathogen in humanized HLA-transgenic mice. The adenovirus reporter system used in our study may serve as simple in vivo method to evaluate future strategies for improving human intrahepatic immune responses in humanized mice.
Hepburn, T. W., et al. (2003). “Antibody-mediated stripping of CD4 from lymphocyte cell surface in patients with rheumatoid arthritis.” Rheumatology (Oxford) 42(1): 54-61. PubMed
OBJECTIVE: Keliximab studies have provided evidence of the therapeutic potential of a non-depleting CD4 monoclonal antibody (mAb) in the treatment of rheumatoid arthritis (RA). Clenoliximab, an immunoglobulin G4 derivative of keliximab, has substantially reduced potential to deplete CD4 cells. In initial studies of clenoliximab, we investigated the hypothesis that the decrease in cell surface CD4 is the result of antibody-mediated stripping from the cell surface. METHODS: Patients received single or multiple intravenous infusions of clenoliximab as follows: 0.05, 0.2, 1, 5, 10 or 15 mg/kg (n=3-5/group); 150 or 350 mg weekly x 4; or 350 or 700 mg every other week x 2 (n=12/group). Blood was collected for up to 16 weeks and pharmacokinetic and pharmacodynamic assessments were conducted using immunoassay and flow cytometry. RESULTS: CD4 count was largely unaffected by clenoliximab treatment. Dose-dependent CD4 coating, down-modulation and stripping were observed. Maximal down-modulation persisted for an increasing period as dose increased, while soluble CD4-clenoliximab complexes accumulated. The amount of CD4 in soluble complex was as much as 20 times the amount of cell-associated CD4. For the same total dose, administration of higher doses, less frequently, resulted in pharmacodynamic profiles similar to those of lower doses administered more frequently. CONCLUSION: Decrease in the density of CD4 on the T-lymphocyte surface is caused by antibody-mediated stripping.